Background Renal impairment (RI) is one of the cardinal features of newly diagnosed multiple myeloma (NDMM), contributing to dismal outcomes and high risk of early death. Improved renal function is associated with prolonged survival for NDMM. The triplet combination of pomalidomide with bortezomib and dexamethasone (PVD) has been proven to be effective in MM patients with RI [1] (The manuscript in preparation). However, the best renal overall response rate (ORR) was 78.8% and 21.2% of patients had no renal response to PVD.
Here we reported an interim analysis to evaluate the renal and hematologic response of SPVD (Selinexor, pomalidomide, bortezomib, dexamethasone) regimen as first-line therapy in NDMM with RI in this prospective, open-label, multicenter, phase 2 study (ChiCTR2200064695).
Methods Eligible NDMM with RI (defined as estimated glomerular filtration rate (eGFR) by MDRD < 40ml/min) were enrolled in the study. Sample size was designed to recruit 62 patients. RI caused by other reasons than tubular nephropathy was excluded. Patients received SPVD (Selinexor 40mg on days 1,8,15, pomalidomide 4mg on days1-14, bortezomib 1.3mg/m2 on days 1,4,8,11, and dexamethasone 20mg on day of and after bortezomib, 21days/cycle) for a maximum of 9 cycles. Autologous stem cell transplantation (ASCT) was administrated after 3 to 6 SPVD cycles for transplant-eligible patients. The primary endpoint was renal ORR at 3 months. Secondary endpoints included major renal response (≥partial response) at 3 months, hematological ORR, minimal residual disease (MRD), progression-free survival (PFS), overall survival (OS), and safety. The definition of both hematological response and renal response was according to the International Myeloma Working Group (IMWG) criteria.
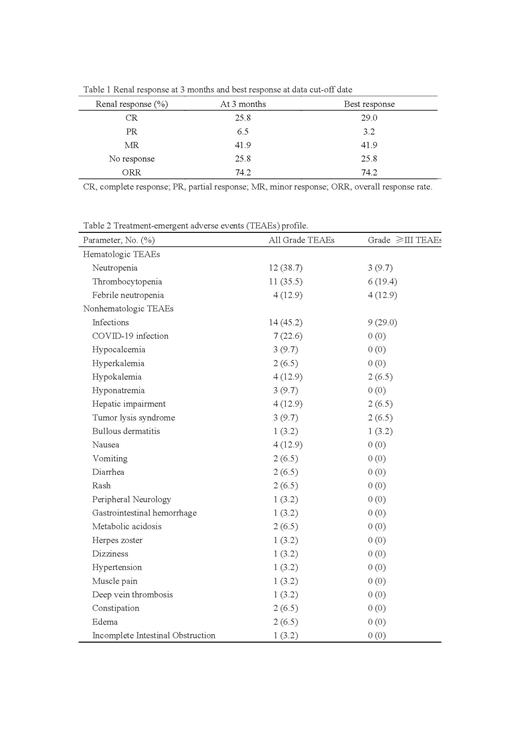
Results Between Oct 28, 2022 and Jun 23, 2023, 31 patients were enrolled across 17 centers, with a median age of 61 years (range: 45-80). The proportion of R-ISS III was 35.5%. Median serum creatine level and eGFR were 365μmol/L [interquartile range (IQR): 214.5-508] and 14.5 mL/min (IQR: 10.5-22.64), respectively. There were 10/31 (32.3%) patients requiring dialysis at diagnosis and 8 patients with high-risk cytogenetic abnormalities [t(4;14), t(14;16), or del(17p)]. At the data cut-off date of July 11, 2023, the median number of SPVD treatment cycles was 3 (range: 1-8). The median follow-up time was 4 months. Two patients received first-line ASCT after induction therapy. The primary endpoint of renal ORR at 3 months was 74.2%, including 6.5% renal PR, and 25.8% renal CR (Table 1). The ORR of the best hematological response was 70.9% (45.1% ≥VGPR, 16.1% CR)(Table 1). The most common treatment emergent adverse events (TEAEs) (incidence >10%) were infection (45.2%), myelosuppression (45.2%), hepatic impairment (12.9%), nausea (12.9%), and hypokalemia (12.9%) (Table 2). Grade 3 or more hematologic toxicity was seen in 35.5% of the patients, the most common being thrombocytopenia (19.4%)(Table 2). Dose reduction or interruption of pomalidomide occurred in 5 patients due to myelosuppression and infection events. Three patients had dose reduction of selinexor due to nausea or vomiting. Notably, among non-hematologic toxicities, 4 patients developed hepatic impairment, and of those, one patient suffered tumor lysis syndrom, hepatic failure and severe infection and then died. Median PFS and OS were not reached.
Conclusion This study demonstrated SPVD is an effective combination in NDMM patients with RI. The toxicity profile was consistent with the reported research, but hepatic impairment during treatment should be noted with caution.
Reference
[1] JIAN Y, CHANG L, SHI M, et al. Renal Response of Pomalidomide with Bortezomib and Dexamethasone in Newly Diagnosed Multiple Myeloma Patients with Renal Impairment: A Prospective, Open-Label, Multicenter, Phase 2 Study [J]. Blood, 2022, 140(Supplement 1): 10167-9. doi:10.1182/blood-2022-159361.
Disclosures
Fu:Takeda Pharmaceutical Company Limited.: Research Funding; Shanghai Changzheng Hospital: Other: WJF is a former staff of Shanghai Changzheng Hospital and now is a staff of Shanghai Fourth People's Hospital affiliated to Tongji University. .

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal